26 Jintana Peesing et al./Research Article:26-32
*Corresponding author:
E-mail: nao.naowarut@yahoo.com
Tobacco smoke pollution from designated smoking rooms in Bangkok’s major
international airport
Jintana Peesing
1
,Naowarut Charoenca
2,3*
,Aungsiri Tipayarom
4
,Nipapun Kungskulniti
2,3
,
Stephen L.Hamann
1
, Siriwan Pitayarangsarit
1
1
Tobacco Control Research and Knowledge Management Center, Bangkok, Thailand
2
Faculty of Public Health,Mahidol University, Bangkok, Thailand
3
Center of Excellence on Environment Health and Toxicology,Bangkok,Thailand
4
Faculty of Science,Silpakorn University,Nakhon Pathom, Thailand.
Abstract
Levels of fine particulate matter with diameters of less than 2.5 microns (PM
2.5
), an indicator of
secondhand smoke, were measured at Bangkok‟s International Airport in: 1) Designated smoking room(s)
(DSR) 2 ( ) just outside these smoking rooms ,and 3( ) in other areas where smoking is prohibited in the
main airport building. TSI SidePak AM 510 monitoring equipment was employed to monitor PM
2.5
for 30
minutes/sample. PM
2.5
samples were taken inside six selected DSR, just outside the same DSR and at
other smoke–free areas inside the building, which included airline lounges, in the walkway to boarding
gates, at arrival waiting areas, and at check–in service areas. The level of PM
2.5
averaged 151.9 µg/m
3
in
smoking rooms, 12.0 µg/m
3
just outside DSR, and 9.0 µg/m
3
in areas where smoking is not allowed.
PM
2.5
values inside smoking rooms were fifteen times the WHO annual air quality standard of 10 µg/m
3
,
whereas the levels outside the DSR were also elevated above the WHO standard. These findings indicate
health risks in smoking rooms for travelers visiting the airport with leakage to areas just outside the DSR.
Results suggest that smoking rooms at the international airport should be removed.
Keywords: Secondhand Smoke(SHS)/Designated smoking rooms(DSR)/Particulate matter/ PM
2.5
1. Introduction
Many large transportation centers for
train, bus, ship and air transport have been smoke-
free for many years (Schmidt, 2007). Despite the
movement to smoke-free transportation centers,
some studies have found lack of action to make
and enforce smoke-free transport centers like in
airports. A recent review of 34 major international
airports in five world regions found that 52.9%
have indoor smoking rooms or smoking areas
(Stillman et al., 2014). Surprisingly, a US study in
2012 in 5 large-hub airports showed high levels of
PM
2.5
, fine particulate air pollution, in designated
smoking room(s) (DSR) at these airports. It was
concluded that DSR pollution from exposure to
secondhand smoke (SHS) in airports poses health
risks for workers and travelers (CDC, 2012). The
study emphasized that restriction of smoking to
DSR is not effective in eliminating SHS. Exposure
to SHS causes all kinds of serious health
consequences, including lung cancer, heart disease
and respiratory infections especially dangerous to
children. Newly added in the latest Surgeon
General‟s Report are conclusions of stroke risk
from SHS exposure: “The evidence is sufficient to
infer a causal relationship between exposure to
secondhand smoke and increased risk of stroke.
The estimated increase in risk for stroke from
exposure to secondhand smoke is about 20–
30%.The evidence is sufficient to infer a causal
relationship between the implementation of a
smoke-free law or policy and a reduction in
coronary events….” According to the 2014 US
Surgeon General report, there is no risk-free level
of SHS; and therefore banning smoking inside is
recommended since not even sophisticated air
cleaning technologies or ventilation systems in
buildings is sufficient. Conventional air cleaning
systems cannot remove all the poisons, toxins,
gases, and particles found in SHS. The only
effective way to protect the health of nonsmoking
employees and travelers from SHS exposure is to
prohibit indoor smoking even in smoking rooms
that are enclosed and ventilated (ASHRAE, 2005;
USDHHS, 2006). Recently, the current US
Surgeon General, Dr. Vivek Murthy, called on the
city of Atlanta, Georgia to make Hartsfield-
Jackson International Airport (ATL) completely
smoke-free (Burress, 2015), when he visited
Atlanta and saw that smoking was allowed in
designated smoking lounges in the airport
terminals. ATL was one of the five airports
studied in 2012; its 13 designated smoking rooms
were designed and constructed by Philip Morris
front groups with the main objective to promote
the social acceptability of smoking (ANR,
2010)(Figure 1).
Thailand has incrementally strengthened
its smoke-free law following findings from
research evidence (Charoenca et al., 2002). As a
result, almost all public places in Thailand are
smoke-free. Recent research has even examined
fine particulate pollution outdoors. For example,
assessment of fine particulate levels in parks in
Bangkok found that levels were quite low, but
differed somewhat by season (Tantadprasert et al.,
2011). The most recent provisions of the Non-
smokers‟ Health Protection Act have been
expanded and include parks and outdoor markets
as well as domestic airports, but still allow
smoking in DSR in international airports (Royal
Thai Government, 2010). In a recent review of

Environment and Natural Resources J. Vol 13, No.2, July-December 2015:26-32 27
smoking policies in airports around the world by Stillman et al. (2014), it was noted that airports
Figure 1: Shocking Difference between this Airport‟s Smoking and Nonsmoking Rooms.
(Source: : http://www.popsugar.com/fitness/Smoking-Room-Washington-Dulles-Airport-37289979)
represent a public and occupational space that is
often overlooked in national or subnational
smoke-free policies. This study was conducted to
assess smoking pollution from airport DSR by
measuring levels of PM
2.5
, respirable particles <
2.5 microns in diameter, a commonly used marker
for SHS (CDC, 2012). It is important to assess
these fine particles since they are usually emitted
in large amounts from burning cigarettes and are
easily inhaled deep into the lungs.
2. Methods
Six of 25 designated smoking rooms at
Bangkok‟s major international airport were
selected and assessed for particulate air levels,
based on their frequency of use. The design of
each room was very similar, with a ventilating fan
in the ceiling. The room sizes were 4m x 5m x
3m, with some chairs in the center of the room,
and one glass door. The sign on the door
indicated that no more than 8 persons be allowed
at a time (Figure 2).
Indoor air quality was assessed by
measuring levels of PM
2.5
, using pre-calibrated
aerosol monitors, TSI SidePak model AM510
(TSI Inc., 2006). The SidePak monitors draw air
through the built-in pump in the device where
particulate matter in the air scatters the light from
a laser. An impactor of <2.5 microns was attached
to the device to measure the concentrations of
PM
2.5
. According to the manufacturer‟s
specifications, the SidePak was zero-calibrated
with a high-efficiency particulate air filter, before
each use; the air sample flow rate was set at 1.7
L/min and set to record the average of PM
2.5
concentrations every minute. In addition, the
number of persons, number of burning cigarettes,
and any activities going on inside DSR were
recorded during the 30 minutes of each sample.
To measure PM
2.5
concentrations inside
and just outside the DSR, two aerosol monitors
were simultaneously used for recording PM
2.5
levels for 30 minutes. Following the protocol
outlined in a previous study by Lee et al., 2010,
one monitor was placed inside the smoking rooms
away from the seats; the other was placed outside
attaching to the wall about 1 foot from the door
and 30 inches from the floor. For comparison,
PM
2.5
samples were collected from other smoke-
free areas inside the airport building, such as
airline lounges, in the walkway to boarding gates,
at arrival waiting areas, airline ticket offices, duty-
free shops, and check-in service areas. Data
collection occurred on 3 days from 8:00 a.m. to
8:00 p.m.

28 Jintana Peesing et al./Research Article:26-32
Figure 2: Typical smoking room in the airport.
3. Results
The 43 samples of respirable particulate
matter were collected from six of the eighteen
DSR and adjacent areas, all were located in the
international zone of the airport. Seven other DSR
in the same building have been closed, as the
current law does not permit smoking in the
domestic section of the airport.
3.1 PM
2.5
results inside, adjacent to, and
distant from DSR
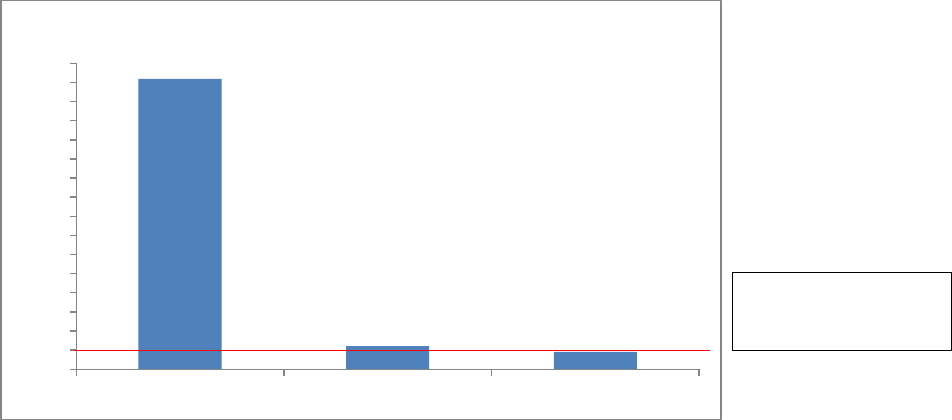
As shown in Figure 3, the mean level of
PM
2.5
inside of the smoking rooms was 151.9
µg/m
3
(range: 29.8 - 488.9). The average PM
2.5
level in areas adjacent to the smoking rooms was
11.9 µg/m
3
(range: 10.2-13.5). The average PM
2.5
level in non-smoking areas in the airport building
was 9.0 µg/m
3
(range: 5.9-10.8). The differences
of PM
2.5
levels measured at all sampling sites were
analyzed using oneway ANOVA. The findings
showed that the average concentration of PM
2.5
inside the smoking rooms was significantly higher
than those of the areas adjacent to smoking rooms
and of the smoke-free areas (p<0.05). As done in
the US 2012 airport study, “smoker density” was
also calculated by dividing the average number of
burning cigarettes by the volume of the DSR. The
association between smoker density and PM
2.5
concentrations was calculated using Spearman‟s
correlation coefficient and found a significant
relationship (rho=0.87; p<0.05). The average
smoker density was 8.3 burning cigarettes per 100
m
3
(range = 2.2-20.0); while the US study found
2.8 burning cigarettes per 100 m
3
(range = 0.3-
9.9). This result demonstrates that levels of tobacco
increased with the number of burning cigarettes. It
was observed that the highest PM
2.5
level (488.8
µg/m
3
) was recorded when the number of burning
cigarettes was the highest (12 cigarettes burnt or
equivalent to smoker density of 20 burning
cigarettes per 100 m
3
). This finding is consistent
with those of Kaufman et.al. (2011) which found
that average increased with the number of lit
cigarettes. Also, peak levels of PM
2.5
were more
than 3 times as high (up to 496 µg/m
3
) when
smoking was present compared to when smoking
was not present. It is important to note that DSR
are heavily used and that the levels of PM
2.5
exposure double at each level from low to high as
shown in Table 1. Even the average calculated
results in low level densities in DSR per 100 m
3
Table 1: Level of Smoker Density in DSR with cigarettes being smoked, calculated smoker densities per
were higher than the average calculated in DSR in the US study (3.0 versus 2.88).100 m
3
and mean PM
2.5
exposure levels
Level of Smoker
Density
No. of DSR with
this level
Range of
cigarettes being
smoked
Calculated
smoker densities
per 100 m
3
Mean PM
2.5
level
Low
4
1.3 - 2.3
3.0
66.55
Medium
14
3.3 – 5.4
7.11
128.16
High
6
7.0 – 12.0
14.7
264.22
Total
24
Ave = 5.00
Ave = 8.3
Ave = 151.9
3.2 PM
2.5
levels compared to the WHO
guideline
When compared to the annual WHO air
quality guideline of 10 µg/m
3
, all samples taken
from inside the DSR and adjacent to DSR were
above this level; whereas PM
2.5
measured from the
Environment and Natural Resources J. Vol 13, No.2, July-December 2015:26-32 29
non-smoking areas were slightly below the guideline as show in Figure 3.
.
Figure 3.Mean levels of PM
2.5
in different locations of the airport.
3.3 Difference of PM
2.5
adjacent to DSR
and in smoke-free areas
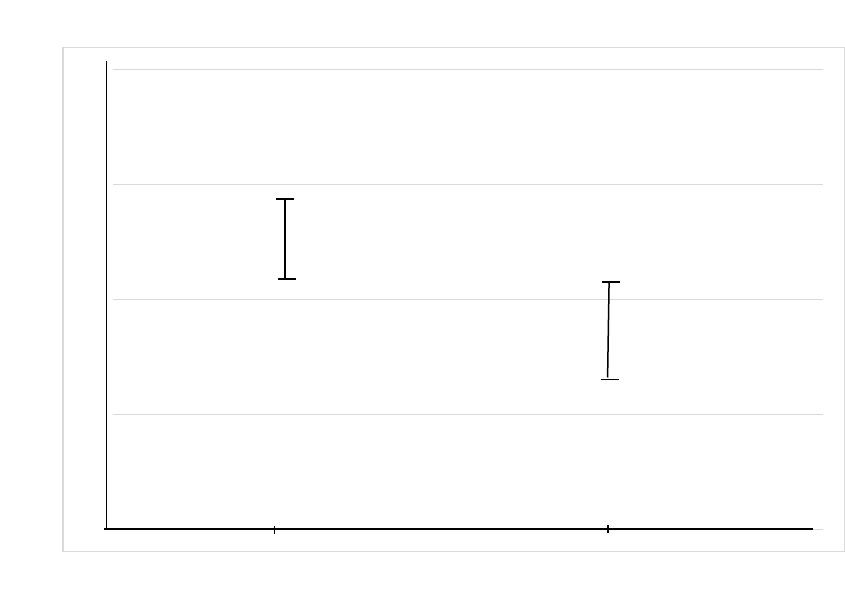
The results in Figure 4 show the
difference of PM
2.5
concentrations measured just
outside the DSR, about 1 foot from the door and
30 inches from the floor (Median = 12.1 µg/m
3
)
and in various non-smoking areas within the
airport building (Median = 9. 5 µg/m
3
). The range
of exposures in the area adjacent to DSR and in
smoke-free areas of the airport are different. The
lowest reading of PM
2.5
from adjacent to DSR
(10.2 µg/m
3
) is little different from the highest
level in relatively smoke-free areas distant from
DSR.(Figure 4).
4.Disscussion
This study was developed and designed
to This study was developed and designed to
determine if levels of PM
2.5
, the most widely used
indicator of secondhand smoke pollution from
smoking, are at levels that could be dangerous to
travelers in Bangkok‟s largest international
airport. PM
2.5
measurement reflects small particles
released from burned materials and cigarette
smoke is the primary source in most public places
like airport locations where cooking is not present.
A comparative study of five large-hub US airports
with designated smoking rooms (DSR) against
four large-hub airports without four large-hub
airports without DSR in 2012 showed very high
levels of PM
2.5
in DSR, elevated PM
2.5
levels
outside DSR, and low levels in the smoke-free
airports. Since airport and DSR conditions vary, it
was important to measure PM
2.5
levels in Bangkok‟s
major international airport to see what exposure
levels are present. A strong feature of this study
was that PM
2.5
measures were taken
simultaneously, so that inside and outside DSR
sampling did not differ in time or place since
multiple sampling instruments were used.
As reported, the mean level of PM
2.5
inside
six DSR tested was 151.9 µg/m
3
, fifteen times the
annual WHO guideline for PM
2.5
exposure. Since
there was a great deal of variability in the
exposure readings, the median score was
somewhat lower (105.7), but still over ten times
the annual WHO guideline. These high levels were
comparable to the mean levels seen in the US
findings inside DSR (151.9 versus 188.7). PM
2.5
levels outside DSR in this international airport
were lower than the means for US airports but still
higher than from smoke-free areas inside the
airport.
Median levels varied by 3 µg/m
3
, but the
variation in range for findings showed that levels
outside the DSR had little variability with the least
level recorded little different than the highest level
recorded from the smoke-free areas in the airport
(10.2 versus 10.8, See Figure 4). Importantly,
PM
2.5
levels outside the DSR were all above the
WHO guideline for annual exposure (10 µg/m
3
)
which reflects a level important for workers
exposed over many working hours throughout the
day and over weeks and months.
Professor James Repace, a health
physicist who specializes in the measurement of
occupational exposure to secondhand smoke
(SHS) and the assessment of the health risk to the
workforce as a consequence of that exposure has
developed analytical models which quantify the
relationship between exposure to secondhand
smoke and mortality. These models have been
validated by other studies where the results have
been consistent with or lower than those
calculated by other health authorities such as the
US Occupational Safety and Health
Administration.
151.9
12.0
9.0
0.0
10.0
20.0
30.0
40.0
50.0
60.0
70.0
80.0
90.0
100.0
110.0
120.0
130.0
140.0
150.0
160.0
Inside DSR Adjacent to DSR Smoke - free areas
PM
2.5
µg/m
3
WHO Air Quality
Guideline =10 µg/m
3
30 Jintana Peesing et al./Research Article:26-32
Figure 4: Maximum ,Median and Minimum scores in a range of multiple measure of PM
2.5
outside DSR
and in smoke-free areas in the airport
They show the relationship of SHS
exposure during one‟s work-life to heart disease
and lung cancer (Repace JL, 2007). Stroke and
other cancers are other conditions not in his
calculations, but which are also linked to SHS
exposure.Stroke is causally-related to SHS
exposure since minor increases of residential
PM
2.5
levels have been associated with clinically
relevant reductions in endothelial function which
adversely affect circulation to the heart and brain.
One study notes, “the change in endothelial
function attributed to a 3 microgram/cu. meter
increase in annual PM
2.5
levels is comparable with
the effect … of smoking or aging by 5 years.”
(Krishnan RM et al., 2012).
Our findings indicated leakage of fine
particles from airport smoking rooms to the
adjacent non-smoking areas. Previous studies have
shown that airport smoking rooms expose non-
smokers in adjacent non-smoking areas due to
leakage of constituents from SHS. Pion and Givel
(2004) demonstrated that significant levels of
nicotine were detected at 35 feet (10 meters) from
an enclosed smoking area that had direct
ventilation to the outside of the airport buildings.
The study was sponsored by the Missouri Group
Against Smoking Pollution Inc. (GASP) to
provide evidence to counter tobacco industry‟s
arguments against making Lambert-St. Louis
international airport completely non-smoking.
There is internal tobacco industry document
evidence that the industry promotes the
construction of DSR and ventilated smoking areas
in airports and has opposed efforts to implement
smoke-free policies in airports (Pion and Givel,
2004; Legacy Tobacco Documents Library, 1990;
Glantz, 2013).
Researchers have concluded that
designated smoking rooms are not able to prevent
tobacco smoke from migrating into the adjacent
non-smoking areas of airport terminals. In another
study conducted at a US medium-sized
commercial airport, it was found that fine particles
from secondhand smoke leaked from smoking
rooms to the surrounding smoke-free areas in the
airport (Lee et al., 2010). In addition, Liu et al.
(2001) reported the leakage of nicotine as
measured from an enclosed smoking area to
adjacent non-smoking areas of California office
buildings. Several studies have provided evidence
that tobacco smoke particles and pollutants drift
from tobacco sources to smoke-free environments
(Brennan et al., 2010; Cameron et al., 2010;
Kaufman et al., 2011; Sureda et al., 2012).
Air contaminants, such as SHS and
particulate matter cannot be removed from
enclosed smoking rooms, even when equipped
with ventilation and air filtration technology.
Even if the room is separately ventilated, the
pumping action of swing doors when they are
opened and closed further enhances tobacco
pollutants leakage from smoking rooms; as much
as 10% of air can leak out to non-smoking areas at
each door movement (Wagner et al., 2004). The
0
5
10
15
20
MEDIAN = 12.06
MEDIAN
= 9.52
10.22
5.93
13.46
10.80
Adjacent to DSR
Smoke- free areas
PM
2.5
Levels
µg/m
3

Environment and Natural Resources J. Vol 13, No.2, July-December 2015:26-32 31
US Surgeon General does not recommend
enclosed smoking rooms at all, but recommends
complete non-smoking in indoor areas to reduce
exposure to SHS, as all poisons, toxins, and
particles found in SHS cannot be removed by any
air cleaning technologies (USDHHS, 2006;
ASHRAE, 2005).
Our findings support other studies that
DSR at the airport is a major source of SHS
exposure for non-smokers in adjacent non-
smoking areas. If airport buildings are not smoke-
free, workers and travelers of all ages are at risk
for SHS exposure. Impact of high PM
2.5
levels
can affect not only smokers who visit DSR, but
cleaning and maintenance staff can have
occupational exposure to SHS (Lee et al., 2010;
Zellers et al., 2007).
Furthermore, children travelling with
adults may be taken inside DSR, or left outside the
smoking rooms. Findings suggest that actions such
as separation of smoking into areas where smokers
are exposed to high levels of particulate material
can be very dangerous to smokers since the
pollutant levels are concentrated to produce an
extremely potent mix of environmental toxicants
that could have sudden and life-threatening
impacts on travelers whose cardiovascular systems
have already become compromised by long travel.
Both extreme high-level exposure for smokers and
lower-level exposure for nonsmokers working in
and around DSR over a working lifetime may be
of concern.
These concerns should foster further
study of both populations since secondhand smoke
can be an added health threat to both smokers and
nonsmoker depending on concentration and
duration of exposure. Study in environments
where exposures are both short- and long-term
could be useful in further characterizing lifetime
threats among various populations and sub-
populations. Smoke-free policies that completely
eliminate smoking inside airports are recognized
as the only way to fully protect the non-smoking
public from SHS exposure (CDC, 2012).
5. Conclusion
In summary, study results point to a
measurable and statistically significant increase in
PM
2.5
levels outside DSR, with dangerously high
levels of PM
2.5
inside the DSR. These levels near
DSR may not be obvious to travelers, but
contribute to health damaging exposures above the
WHO annual standard for particulate matter in
ambient air.
Results of this study should lead to
review of present Thai legislation so that
international airports are included as smoke-free
as with domestic airports. Further studies of
tobacco smoke exposure may benefit from using
other indicators of SHS to characterize cigarette
smoke exposure using nicotine samplers to
complement PM
2.5
measures.
6. Acknowledgement
Funding and support for this study was
provided by the Tobacco Control Research and
Knowledge Management Center. Cooperation
from airport authorities is also acknowledged and
was crucial in locating and monitoring designated
smoking rooms in use in the airport at the time of
this research.
7. References
American Society of Heating, Refrigerating, and
Air Conditioning Engineers 2005 ASHRAE’s
Environmental Tobacco Smoke Position
Document Committee, “ASHRAE Position
Document on Environmental Tobacco Smoke,”
June 30, 2005.
ANR. Americans for nonsmoker‟ rights. 2010.
Smoking policies in the 30 busiest US airports.
July 5, 2010. Accessed on September 28, 2015 at:
http://www.no-smoke.org
Brennan E, Cameron M, Warne C, et al. 2010
Secondhand smoke drift: examining the
influence of indoor smoking bans on
indoor and outdoor air quality at pubs and
bars. Nicotine Tob Res,12(3):271-7. doi:
10.1093/ntr/ntp204.
Burress, J. 2015 Surgeon General Calls Out
Atlanta Airport's Smoking Lounges. NPR
Station, WABE, Atlanta, Georgia. May 18,
2015. Accessed on September 28, 2015
at: http://wabe.drupal.publicbroadcasting.net/
post/surgeon-general-calls-out-atlanta-airport-
s-smoking-lounges
Cameron M, Brennan E, Durkin S et al. 2012
Secondhand smoke exposure (PM
2.5
) in
outdoor dining areas and its correlates. Tob
Control, 2(19):19-23
Centers for Disease Control and Prevention 2012.
Indoor Air Quality at Nine Large-hub
Airports with and without designated smoking
areas – United States, October-November
2012. MMWR, 61:1-5.
Charoenca N, Kungskulniti K, Hamann SL, et al.
2002 Exposure levels of carbon monoxide and
nicotine at restaurants and nightclubs in
Bangkok. Bull Health Sci Tech, 5(2):115-24.
Glantz SA. 2013 Israel is failing to protect its
citizens from secondhand smoke : underestimating
public support. Israel Journal of Health Policy
Research, 2(1):24
Kaufman P, Zhang B, Bondy SJ, et al. 2011 Not
just „a few wisps‟: real-time measurement of
tobacco smoke at entrances to office
buildings. Tob Control, 20(3):212-18. doi:
10.1136/tc.2010.041277
Krishnan RM, Adar SD, Szpiro AA, et al. 2012
Vascular responses to long- and short-term
exposure to fine particulate matter: MESA Air
(Multi-Ethnic Study of Atherosclerosis and
Air Pollution). J. Am. Coll. Cardiol, 60(21):
2158–2166. doi: 10.1016/j.jacc.2012.08.973
Lee K, Hahn EJ, Robertson L, Whitten L, Jones
LK, Zahn B. (2010). Air quality in and around
32 Jintana Peesing et al./Research Article:26-32
airport enclosed smoking rooms. Nicotine
Tob Res, 12(6):665-668.
Legacy Tobacco Documments Library.1990.
Airport strategy plan, 1990. San Francisco,
California: University of California, San
Francisco. Accessed on September 28, 2015
at http://legacy.library.ucsf.edu/tid/ajm30c00.
Liu KS, Alevantis LE, Offermann FJ. 2001. A
survey of environmental tobacco smoke
controls in California office buildings. Indoor
Air, 11(1):26-34.
Pion M, Givel MS. 2004. Airport smoking rooms
don‟t work. Tob Control, 13(Suppl I):37-40.
doi:10.1136/tc.2003.005447
Repace JL. 2007 Exposure to secondhand smoke.
In: Ott WR, Steinenmann AC, Wallace LA,
eds. Exposure Analysis. Boca Raton,
Louisiana: CRC Press, 201-235.
Royal Thai Government.2010 Nonsmokers’
Health Protection Act: Notification 19.
Bangkok: Royal Thai Government.
Schmidt CW. 2007 A change in the air: Smoking
bans gain momentum worldwide. Environ
Health Perspectives Aug;115(8):A412-A415.
See the Shocking Difference Between This
Airport's Smoking and Nonsmoking Rooms.
(April 16, 2015).Available at:
http://www.popsugar.com/fitness/Smoking-
Room-Washington-Dulles-Airport-37289979.
Accessed on December 11, 2015.
Stillman FA, Soong A, Kleb C., et al. 2014. A
review of smoking policies in airports around
the world. Tob Control Published Online First:
March 17, 2014 doi:10.1136/tobaccocontrol-2013-
051364.
Sureda X, Martinez-Sanchez JM, Lopez MMJ, et
al. 2012 Secondhand smoke levels in public
building main entrances: outdoor and indoor
PM
2.5
assessment. Tob Control, 21(6):543-
48. doi: 10.1136/tobaccocontrol-2011-050040
Tantadprasert A, Nutmagul W, Uyasatian U, et al.
2011 Ambient TSP and PM
10
concentrations
in public parks in Bangkok, Thailand. Env
and Natural Res J. 9(1): 24-30.
TSI Incorporated. 2006. Model AM510 SidePak
Personal Aerosol Monitor User Guide.
Shoreview, Minnesota, USA
U.S. Department of Health and Human Services.
2006.The Health Consequences of
Involuntary Exposure to Tobacco Smoke:
A Report of the Surgeon General. Atlanta,
GA: US Department of Health and Human
Services, Centers for Disease Control and
Prevention, Coordinating Center for Health
Promotion, National Center for Chronic
Disease Prevention and Health Promotion,
Office on Smoking and Health.
U.S. Department of Health and Human Services,
Centers for Disease Control and Prevention,
National Center for Chronic Disease
Prevention and Health Promotion, Office on
Smoking and Health. 2014 The health
consequences of smoking – 50 years of
progress: a report of the Surgeon General.
– Atlanta, GA..
Wagner J, Sullivan DP, Faulkner D , et al. 2004.
Environmental Tobacco Smoke Leakage from
Smoking Rooms. Journal of Occupational
and Environmental Hygiene, 1(2):110-118
Zellers L, Thomas MA, Ashe M. 2007. Legal
Risks to Employers Who Allow Smoking in
the Workplace. Am J Public Health, 97(8):
1376-1382. doi:10.2105/AJPH.2006.094102
